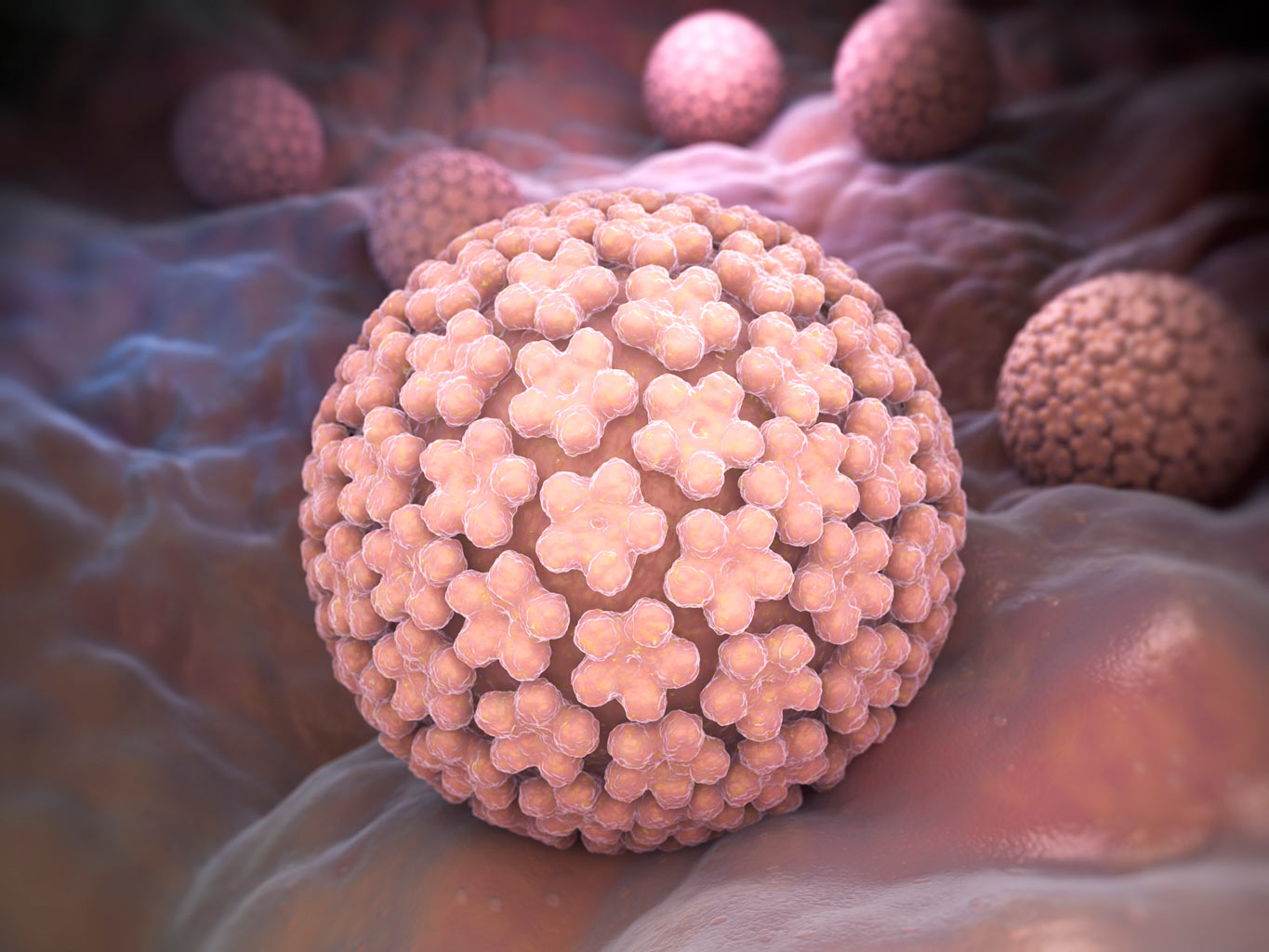
What is HPV?
HPV stands for the human papillomavirus. There are over 100 kinds of HPV, most of which cause no health problems. Many of you may be familiar with common warts that appears on hands and feet. These are not sexually transmittable. However, about 40 strains of HPV can infect the genital region (scrotum, penis, anus, rectum, cervix, vulva, and vagina.) They can also affect a person’s throat and mouth. Of those HPV strains at least 14 are known to be high risk or cancer causing. Genital warts (condyloma acuminatum) can be raised, flat, shaped like a cauliflower, be small or large, and typically display as a bump or group of bumps in the genital region.
How is HPV transmitted?
HPV can be transferred via skin to skin contact. It is the most common sexually transmitted disease (STD) and is often transmitted through oral, vaginal, or anal sex. Both men and woman can spread the virus with or without the display of symptoms. Many may never know they ever had the disease.
Even if you have only had sexual contact with one person, anyone who is sexually active is susceptible to HPV. The virus can lay dormant for weeks, months, and even years, making it hard to know when infection occurred or if you have spread the virus to others.
Preventing and Reducing the Risk of HPV

Genital HPV infections are very common. In fact, most people who have sex will get HPV at some point in their lifetime. According to the Center for Disease Control (CDC), around 79 million Americans are infected with HPV (1). With that said, there are things you can do to decrease your chances.
Use Condoms and Dental Dams
While condoms and dental dams will not completely protect from skin to skin contact, they can reduce your chances of getting HPV.
Routine Screening for Cervical Cancer
It is important that woman get routine screening from their health care providers. Those with high risk type HPV often never show signs of the infection until serious changes have already occurred. Pap tests can help catch any cellular changes that may be occurring so that treatment can begin as soon as possible. In addition, your doctor may notice changes in color, thickness, pain, discharge, or bleeding that may signal signs of cancer.
Penile and anal cancer is possible in men. Therefore it is important men receive routine screening so that any changes can be detected and addressed right away. Genital warts are considered low risk and do not lead to cancer. However, they can cause discomfort, are transferable to others, and should be treated.
Abstinence or Mutually Monogamous Relationships
Having no sexual contact or having sex only with someone who has sex with you decreases your odds of contracting HPV. Unless you have genital warts or high risk HPV, you’ll probably never know you had HPV.
HPV Vaccine
While the vaccine does not prevent against all strains of HPV, it can help reduce the risk of contracting certain types of HPV that can lead to a higher risk of genital warts and cancer. In particular, the two main types (16 and 18) that cause 80% of cervical cancers, and types 6 and 11, which lead to 90% of genital warts. Talk to your doctor to see if you are a good candidate for the HPV vaccine as well as the associated risks. (2)
HPV and Cancer
In most cases, HPV goes away on its own and does not cause any health problems. Without treatment, most cases clear the body on their own and about 90 percent of cases clear within 2 years. (3) However, there are certain strains of HPV that can increase the risk of developing penis, anal, vulva, vaginal, and cancers in the throat, tongue, and tonsil region (oropharyngeal cancer). While there is no known cure for HPV at this time, cancers typically takes years to develop and any cellular changes can often be detected and treated before they become cancer. Therefore it is important to get regular screening and checkups.
If an HPV test comes back positive, knowing this allows you to work closer with your doctor. In particular, with any abnormal Pap smear or if high risk HPV is detected, your doctor may perform a colposcopy (a procedure that looks for precancerous cells on the cervix), cryotherapy (a treatment that removes precancerous cells through a freezing method), or a Loop Electrosurgical Excision Procedure, also known as LEEP (a procedure to remove precancerous cells using an electrical current).
Likely the frequency of screening will increase, at least for a period of time. This does not mean you have cancer but you are at an increased risk for getting cancer in the future. The goal is to make sure you stay healthy and cancer free.
HPV and Pregnancy
In most cases, HPV will not impact the developing fetus in any way. If you have had genital warts or high risk HPV, inform your health care provider. It is possible for warts to bleed during delivery and they may need to be removed prior to giving birth. In some circumstances, a cesarean section may be needed. Very rarely are warts transferred to the infant during vaginal birth. In rare cases, non-cancerous warts have been transmitted to the newborn’s throat. In these cases, your doctor can help determine what treatment is necessary, if any. (4,5)
Those who have had cervical tissue removed can deliver preterm or at lower birthrates. However, many women continue to have healthy and normal births and pregnancies regardless of previous treatment. Make sure to talk to your pregnancy team regarding the treatments and procedures you may have had so that they can help educate you and design a plan specific to your body and your situation. With the right pregnancy team, many of these women continue to have healthy babies without complication (6).

In any sexual relationship it is important to be open and honest with your partner. Having conversations about past sexual relationships, STDs, getting tested for STDs, and birth control methods are all vital to a healthy relationship. If you have been diagnosed with HPV, don’t be embarrassed or ashamed. What matters is that you stay healthy and get the care you need.